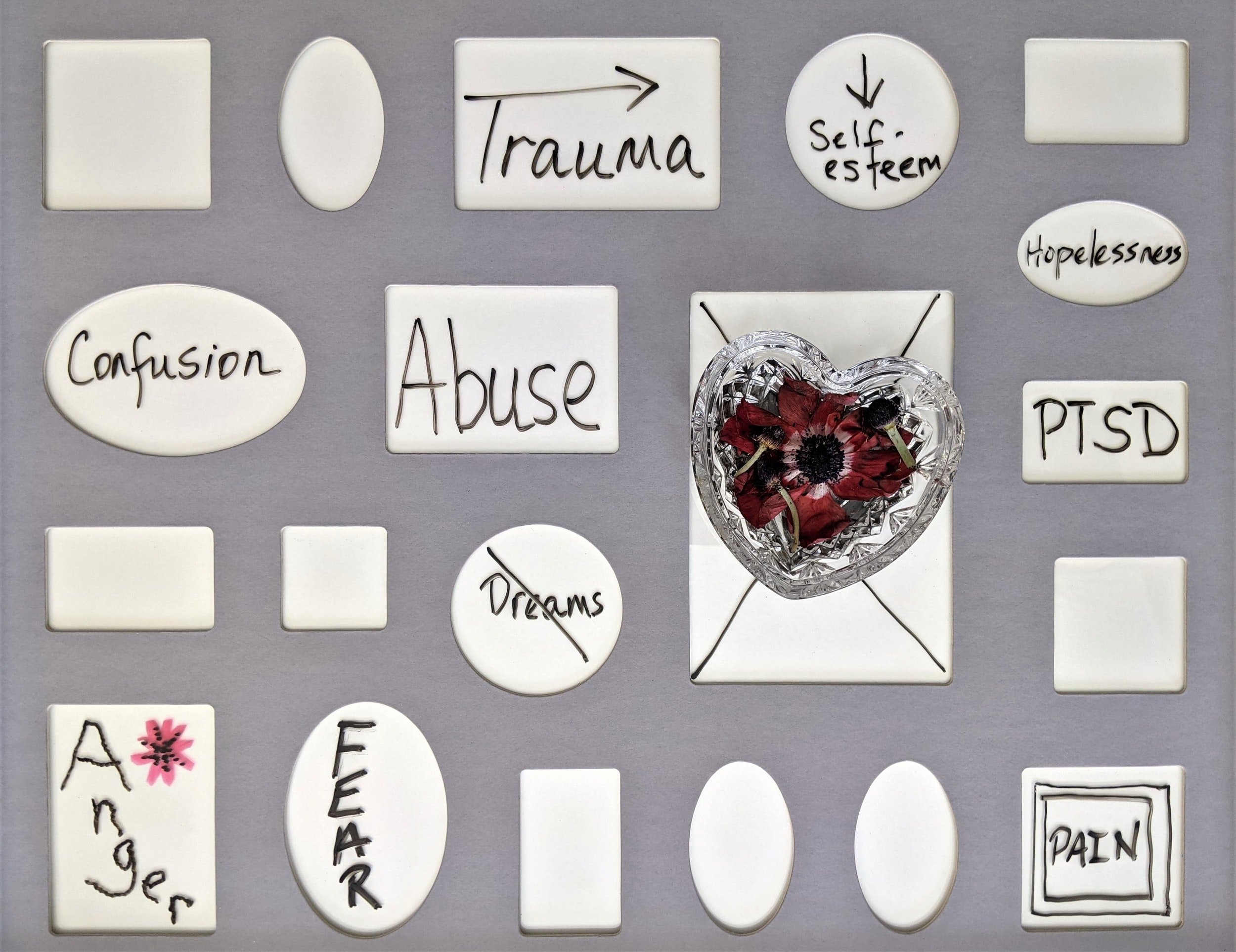
Post-Traumatic Stress Disorder
Most of us have had frightening experiences. Often we think about them long after the event. For some people, these distressing thoughts or images persist, as well as other symptoms such as a strong sense of threat, feeling emotionally numb, and irritability. If these reactions occur frequently, last at least a month, and interfere with daily functioning, the person may be suffering from PTSD.
What are the symptoms of PTSD?
PTSD symptoms for adults, adolescents, and children older than six; symptoms must persist for more than one month:
At least 1 of:
Intrusive thoughts or images about the event.
Dreams or nightmares about the event or similar events.
Flashbacks or illusions about the event (children may act out the event in play).
Distress when reminded of the event.
Physical arousal (becoming physically upset) when reminded of the event.
At least 1 of:
Avoidance of thoughts or feelings associated with the event.
Avoidance of reminders of the trauma (people, places, activities, objects, or situations).
At least 2 of:
Inability to recall important aspects of the event (not explained by loss of consciousness).
Ongoing negative beliefs and expectations about oneself (e.g., “I am bad”) or the world (e.g.,
“The world is a very dangerous place”).Unnecessarily blaming self or others for causing the traumatic event or for consequences.
Persistent negative trauma-related emotions (e.g., fear, horror, anger, guilt, or shame).
A decreased interest in previously significant/enjoyable activities.
Feeling detached/alienated from others.
Restricted emotions (e.g., persistent inability to experience positive emotions).
At least 2 of:
Irritable or aggressive behaviour.
Self-destructive or careless behaviour.
Hypervigilance (always on guard).
Exaggerated startle response (too easily startled or scared).
Difficulty concentrating.
Changes/disturbances in sleep (e.g., insomnia).
What do we know about PTSD?
Research shows us that the majority of people exposed to a traumatic event experience some symptoms of PTSD within the first weeks and most people’s symptoms start to go away within one month. Twenty to forty percent suffer from PTSD for at least a month, one-half to two-thirds of those initially distressed people recover within the first year, and the rest remain disabled for more than one year. Research with transportation and assault victims, for example, suggests that between 10 and 20 percent are disabled for several years.
PTSD is not limited to combat and disaster experiences. It also occurs following sexual or physical assault, transportation or industrial accidents, life-threatening illnesses such as cancer, war-zone experiences, and repeated exposure to others’ physical trauma (e.g., emergency room nurses and ambulance attendants). Roughly speaking, sexual and physical assault results in the highest rates of PTSD, exposure to life-threatening illness (e.g., breast cancer) result in the lowest rates, and transportation and industrial accidents are in between.
It was initially assumed that the more severe the initial stress, the more likely an individual would develop PTSD. However, that assumption has not been supported by research. The severity of trauma (e.g., damage to car, physical injuries during assault) is less important in predicting PTSD than is the survivor’s initial emotional response. PTSD is more likely to occur to people whose initial responses include extreme fear, panic attacks, or dissociation (a method of coping by blocking out of one’s mind the upsetting event as it is occurring). Some people are more vulnerable than others, especially those with a history of depression, anxiety, or other traumas, an angry disposition, or a style of coping with stress that includes not thinking about or
talking about the event (an avoidant style). Women are about twice as likely to develop PTSD as men. People’s subsequent attitudes and beliefs about their personal safety can influence recovery. That is, negative beliefs about one’s own coping ability or the safety of the world, as well as repeated angry or resentful thinking about the reasons for the trauma all make it harder to recover. There is increasing evidence that traumatic experiences result in cumulative psychological distress. Emergency workers (e.g., paramedics, police) are also made more vulnerable by relative deficits in organizational support.
PTSD can result in significant personal suffering. Avoidance of important activities (e.g., driving a car, socializing with others) decreased sleep and related fatigue, and interference with one’s relationships are some of the more typical consequences. These problems can have significant financial costs to the
individual and society. PTSD is associated with subsequent physical health difficulties (e.g., headaches), resulting in increased medical care and absenteeism from work or school. PTSD sufferers are more likely to be unemployed and have lower incomes than similar persons without PTSD.
Effective assessment and treatment of PTSD
Two important issues interfere with the accurate assessment of PTSD. First, many cases of PTSD are missed because health professionals fail to ask patients if they have experienced traumatic events (e.g., sexual assault). It is important for health practitioners to ask patients and it is vital that patients tell health practitioners about traumas in their lives. On the other hand, many health professionals overdiagnose PTSD in cases where they focus solely on "classic" symptoms (e.g., nightmares) rather than conducting a systematic diagnostic interview. Effective assessment of PTSD requires detailed screening for traumatic stressors and a systematic diagnostic interview. Specialized psychological tests such as the Stressful Life Events Screening Questionnaire (SLESQ), Posttraumatic Diagnostic Scale (PDS), PTSD Checklist (PCL), Posttraumatic Cognitions Inventory (PTCI), and Accident Fear Questionnaire are frequently helpful both for diagnosis and for treatment planning.
Over the past decade, psychologists have evaluated treatments for PTSD. Some have proven to be quite effective, while others have not. The popular one-session procedure referred to as Critical Incident Debriefing now appears to be of little benefit in reducing psychological distress. However, brief cognitive-behavioural therapy (5-6 sessions) provided to very distressed people shortly after a traumatic event appears helpful in reducing PTSD symptoms. Short-term (8-30 hours) behavioural and cognitive therapies have been shown to alleviate PTSD symptoms in chronic sufferers. Common therapeutic components of successful treatments include giving people the opportunity to repeatedly describe the traumatic event and their emotional responses to it, writing assignments about how they feel about the event and what it means to them and repeated opportunities to discuss the trauma and what it means. Helpful stress coping skills include helping patients to examine beliefs about personal safety (e.g., "I can never be safe again"), the gradual re-establishment of more realistic boundaries of safety (e.g., It is safe to go into tall buildings again"), and relaxation training. In order to receive the treatments described above, you can visit a qualified mental health professional such as a psychologist.
While many people can be treated effectively with these therapies, there are still a number of PTSD sufferers who fail to respond to treatment. Individuals with chronic physical pain, those with severe depression, and those who are very angry about their traumatic event are all less likely to improve. The development of new multi-component treatments for PTSD and its complications is now ongoing. For example, researchers are evaluating the usefulness of combining anger management training and behaviour therapy for depression with standard PTSD treatments.
Pharmaceutical treatments for PTSD are in the early stages of evaluation. At this time, it appears that some of the more recently developed anti-depressant medications may benefit trauma survivors by reducing concurrent symptoms of depression or muting the hyperarousal symptoms of PTSD. Consult with a health professional about this treatment option.
Canadian Psychological Association - Fact Sheet: Post-Traumatic Stress Disorder